Support the next generation
Help us support our future leaders with a gift to this endowed diversity scholarship.
GIVE NOW >Serving MD, MD/PhD, Res., Fel., PhD, PA-C (MEDEX), MA, MS, BS, PT, OT and P&O alumni, your UW School of Medicine Alumni Association is the place to connect with your classmates, your School and the next generation of medical professionals.

850 Republican Street, C-5
Seattle, WA 98195-8045
 Fall marks the start of school, and this year, school looked a little different for medical students at the UW School of Medicine.
Fall marks the start of school, and this year, school looked a little different for medical students at the UW School of Medicine.
The School has adopted a hybrid model where any classes that can be online are online, and formats like labs and clinical skills training, where in-person learning is essential for a medical student’s foundation, are in person.
“With the caveat that across the six campuses things might look different and, depending on the location, people might not be able to learn in person,” says Suzanne Allen, MD, Vice Dean, Academic, Rural & Regional Affairs.
The School sees flexibility as a necessity — as it is for all plans in 2020.
“There could be a surge in cases at any campus at any time, a primary care office might say no to having students in clinic based on the numbers of COVID-19 cases, or students or faculty might need to quarantine,” says Allen. “We are hopeful these classes can be in person, but they might need to do things remotely.”
The School is ready should some campuses or students need to move their schedule online.
An unusual year: spring through fall quarter 2020
“Thinking back to March, we had students asking to get out of clerkships,” says Allen. “Everyone was so panicked because there was so much that we didn’t know at that time: does everyone need an N95 or are cloth masks OK?”
Since then, from a procedural standpoint and from a daily life standpoint, so much has changed.
With Western Washington being the epicenter of the pandemic in March, all students in the Foundations phase (classroom-based learning) were moved online and shortly after the School decided to pull students in clerkships out of their in-person rotations. This was right before the Association of American Medical Colleges (AAMC) released their own guidelines and medical schools all over the country paused their clinical rotations. In April, the School made the decision not to return to clerkships until summer quarter.
At the end of June, the start of summer quarter, students returned to their clerkships. Allen reports that things went really well.
“UW Medicine has done a good job of putting processes in place to keep everyone safe and able to learn,” says Allen. “It was a huge effort to redo schedules and ensure that everyone could move forward and stay on time to graduate. Our faculty have been amazing and have put in hours of work to get everything ready for students to have virtual education and distance education.”
To keep students on track to graduate, in-person Patient Care Phase clerkships were cut by a third for the 2020-2021 Patient Care Phase. Although cutting valuable clinic time isn’t ideal, it is still important that students are able to practice their clinical skills in person.
To support laboratory learning, the School has reduced the amount of people per lab and increased the amount of sections.
Prioritizing laboratory and clinical classes for in-person learning, breaking down anatomy lab sections into smaller groups, reducing clerkship requirements, teaching core courses online and having a flexible attitude are important steps forward.
What to expect: winter and spring quarter 2021
Allen anticipates that during winter quarter, the Foundations Phase will be taught in a similar, hybrid-presentation format and clinical skills and anatomy courses will be in person.
“Everyone is anxious that we could be back to in-person classes soon,” says Allen. “I think we will be doing the same thing in spring quarter and potentially next fall. We would need herd immunity to start gathering in large groups again and I don’t think we’ll be at that point by spring quarter.”
A shifting future for medical schools
A few things have changed in medical education across the country since the pandemic began, says Allen. For starters, how people apply to residency programs.
“Most students do 12 to 15 interviews for residency, which is a lot of travel around the country,” says Allen. “This year they are doing virtual interviews and, from the standpoint of the students, it is a lot less expensive and doesn’t take up as much time.”
Allen adds that the downside of virtual interviews is not getting a good feel for the community you’re visiting.
“Our UW School of Medicine alumni association is great and is offering prospective students the opportunity to talk and get a sense of the community,” says Allen.
The School has also started doing virtual medical school interviews and has made the Medical College Admission Test (MCAT) optional for 2021.
Although it’s unknown what changes will stick as status quo for medical schools or even what next semester holds, students and educators alike are learning valuable lessons in resilience.
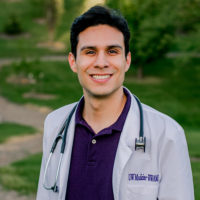
Eli Luna is a third-year UW School of Medicine student who is part of the Idaho WWAMI cohort and the first recipient of the Committee for Minority Faculty Advancement Endowed Diversity Scholarship. Just as he was about to begin clinical rotations, all of his plans changed with the arrival of COVID-19.
I was scheduled to take my medical licensing exam mid-March, when I received an email from the test administrators telling us that all testing sites would be closed until further notice. For one month, I didn’t know when I was going to take my test. Just prior, the UW School of Medicine had announced that they were going to postpone all clinical rotations. There was talk among us students that we might have to delay our graduation.
Then the School re-opened clinical rotations in June, but many sites were still closed due to COVID concerns and lack of PPE. For this reason, the School trimmed some rotations from six weeks down to four, so we could complete all of our requirements and still graduate on time — a relief to hear!
But it’s been challenging. Normally, the first week of a new rotation is spent getting to know the medical system and the people in the hospital. Now, introductions are kept to a minimum; we jump right into learning. After all, we still have to cover the same amount of material, just in less time. That means I sometimes come out of the clinic after 10 to 12 hours and immediately start studying. So there’s an added stress.
My schedule has also completely changed from what I thought it was going to be. Instead of starting my rotations in April, I started in July with another student in Whitefish, Montana. The clinic had never had two students at the same time before the summer of 2020, so they had to find new preceptors and re-arrange their schedules as well.
Now, I’m heading to Spokane, somewhere I didn’t expect to be going. Although this is not where I originally was scheduled to have one of my rotations, I am grateful that the School found a different rotation within the same specialty to make up for it. As medical students, we’re gaining real-time experience learning how to adapt to a pandemic and a changing medical system.
I’m learning from this experience in other ways, too. COVID has exposed a lot of inequities that have always been there for minorities within our healthcare system. If anything, this has increased my drive to serve the Hispanic community. I see so many needs — whether for translation services or transportation services. It’s inspired me to do more for this population.
By Katherine Brooks and Eleanor Licata